In Some Medical Deserts, Pharmacists Alone Provide Healthcare
Healthcare deserts come in many forms. There are shortage areas for primary care, dentists, pharmacists, and trauma centers, to name a few. Here, we mapped the ratio of primary care doctors to pharmacists across the continental U.S. The map represents the opportunity for pharmacists to help fill a need in the country’s healthcare network, reducing medical deserts.

The sprawl of medical deserts is advancing. Nearly 30% of people in the U.S. live in areas where there are not enough primary care doctors for the population who needs them, and that’s just one measure when considering healthcare deserts. There are also places and populations experiencing a deficiency of hospitals, trauma centers, specialists, pharmacies, dentists, mental health services and more.
The ongoing physician shortage, which is one of the healthcare workforce shortages tracked by the U.S. governmentWorkforce Shortage Designations, Health Resources and Services Administration, August 2022, is only expected to worsen as more doctors are absorbed into hospitals or retire, with a deficit of 139,630 such providers projected by 2030.Physician workforce in the United States of America: Forecasting nationwide shortages," Feb. 6, 2020, Human Resources for Health
The data trendline across geographic areas is clear: The number of primary care shortage areas as of Sept. 30, 2022 increased 15% to 7,447 from September 2016 to September 2022.U.S. Department of Health and Human Services Fact Sheet, Sept. 30, 2022 These federal designations can be geographic places like counties, cities and census tracts, or they can be populations or facilities.
Many of these places, however, do have another care provider: a pharmacist.
In this data dive, we mapped the relative number of pharmacies compared to primary care providers in each ZIP code, represented as a ratio. The resulting visualization, where pink areas mean more pharmacies and orange means more providers, represents the benefit many communities could realize in relying on their pharmacists for more than just dispensing medications.
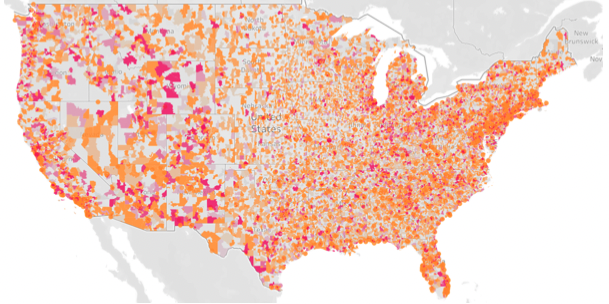
• Pink: Many pharmacies compared to providers • Orange: Many providers compared to pharmacies
Sources: National Plan and Provider Enumeration System, National Council for Prescription Drug Programs
Why pharmacists are uniquely positioned to help
The COVID-19 pandemic accelerated the growing role of pharmacists as more fully functioning members of the patient care team. According to the 2022 CoverMyMeds Medication Access Report, 77% of patients received COVID-19 vaccinations from a pharmacist, and 39% received a vaccination other than COVID-19 from a pharmacist. More than half, 52%, of patients said their relationship with their pharmacist changed in 2021, with more advising and services unrelated to medication coming into play.
Pharmacists enjoy their growing role, with 72% saying counseling patients on their conditions was fulfilling or very fulfilling, according to the Medication Access Report.
But the opportunity to practice at the top of their license, as it is said in the industry, is cloudy for pharmacists. They aren’t recognized as medical providers by Medicare and are unable to bill for the non-medication services they can provide according to their training.Billing and Payment Center, American Pharmacists Association, 2021
Pharmacists are in a good position — with regard to physical location and otherwise — to provide care beyond dispensing medications. Patients trust the guidance they receive from pharmacists, with 90% saying they would follow advice and recommendations from pharmacists.2021 Health Care Insights Study, CVS Health
And pharmacists’ availability in many places — though they’re not accessible everywhere, to be surePharmacy Deserts Disproportionately Affect Black and Latino Residents in Largest U.S. Cities, May 3. 2021, University of Southern California Schaeffer Center for Health Policy & Economics — rates high on patients’ list of important attributes when choosing care. Ease of access to care and having providers close to home or work were the most important factors for 89% and 85% of patients, respectively, responding to a recent survey.2021 Health Care Insights Study, CVS Health
Change is on the way for pharmacists’ role as members of the care team. As legislation advances in states across the country, they are increasingly gaining the ability to be paid as providers for certain services.2022 Provider Status Midyear Legislative Update, National Alliance of State Pharmacy Associations, Aug. 25, 2022 Most often, those services include strep testing and diagnosis, expanded immunizations, prescribing and dispensing hormonal contraceptives including birth control injections, and administering HIV treatments and counseling patients.
There is also movement at the federal level to further pharmacists’ role as care providers. Federal barriers can hinder pharmacists’ ability to meet patients in their communities, whether with remote care or in-person care. State efforts are a patchwork that can be confusing. Federal legislation such as HR7213, the Equitable Community Access to Pharmacist Services ActGovInfo page for HR7213, Equitable Community Access to Pharmacist Services Act, March 2022, can address law limitations, helping patients access essential care and services provided by pharmacists.
Better recognition of pharmacists as integral members of the care team can help solve physician workload challenges and the primary care shortage that’s growing each year. They are well-positioned to help fill the gaps in the U.S. healthcare network, shrinking medical deserts.
For more insights on how healthcare is changing for patients, providers and pharmacists, visit the 2022 CoverMyMeds Medication Access Report.
The latest healthcare insights, floated right to your inbox.





